In Vitro Fertilization
In Vitro Fertilization
In vitro fertilization (IVF) techniques are complex procedures that involve the fusion of the egg and sperm in a laboratory. They are performed by extracting the eggs from the ovarian follicles through a puncture, previously stimulated, and combining them in the laboratory with the selected sperm from the semen sample. As with artificial insemination, we can distinguish two types depending on the semen used:
- In vitro fertilization with the couple's semen
- In vitro fertilization with donor semen, provided by a sperm bank.
It is important to note that even if non-anonymous donor sperm is used, when both members of the couple undergo assisted reproduction treatments and sign the informed consent, the children born from these treatments will be the legitimate children of both. The same applies to the use of non-anonymous donor eggs. Considering the technique used to perform the fertilization in the laboratory, we can distinguish two types of techniques, which will be discussed in detail later:
- Conventional in vitro fertilization: Commonly called IVF. It involves combining an egg with a group of sperm and waiting for them to fuse on their own.
- Intracytoplasmic Sperm Injection: Known by the acronym ICSI. It involves the microinjection of a single sperm into the egg.
 "The choice of one of these techniques will depend on the couple's subfertility conditions, as well as their reproductive history and the experience of each center."
"The choice of one of these techniques will depend on the couple's subfertility conditions, as well as their reproductive history and the experience of each center."
However, the steps to follow are the same in both techniques:
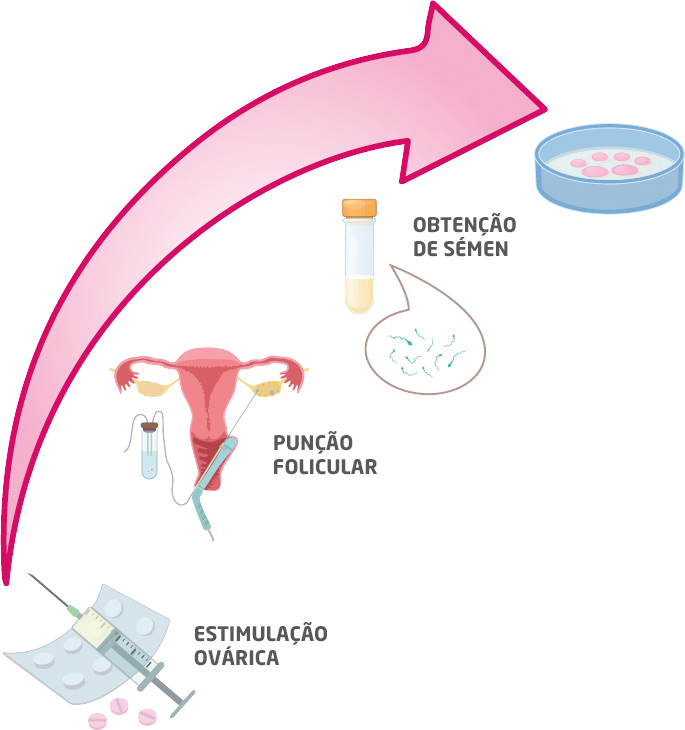
Ovarian stimulation: The goal is to achieve the maturation of a sufficient number of eggs according to the ovarian response of each patient through the administration of medication. This medication is very easy to administer, it is a subcutaneous injection per day (like insulin in diabetic patients). This stimulation usually lasts about 10 days and generally requires about 3 ultrasound control exams. When the ideal follicular size is reached, ovulation is triggered by an hCG injection, and the follicular puncture is scheduled about 36 hours after the injection.
Follicular puncture: It involves the extraction of the eggs produced in each ovary through a vaginal puncture guided by ultrasound. It is performed with sedation for better recovery, so fasting is required. Usually, the day after the puncture, progesterone treatment is started, and folic acid is also recommended.
Semen collection: On the same day as the puncture, a semen sample will be collected for in vitro fertilization. Generally, the sample is collected by masturbation in a room designated for this purpose. Additionally, the semen can come from previously frozen samples, both in the case of donor semen and if it was previously preserved for various reasons.
In special cases, due to different fertility problems, sperm are obtained from the epididymis or by testicular biopsy. These last two procedures would be performed in the operating room by a urologist. It is an invasive procedure performed when:
- No sperm are found in the ejaculation.
- Certain anomalies are detected in the sperm.
- There is an obstruction in the vas deferens.
- The man has undergone a vasectomy.
Testicular biopsy is a technique that involves surgically extracting a small sample from the testicle and checking in the laboratory for the presence of sperm to be used in the in vitro fertilization process.
Semen preparation: Once the semen sample is collected, it is processed in the andrology laboratory, the seminal plasma is removed, and the best sperm are selected to be used for in vitro fertilization.
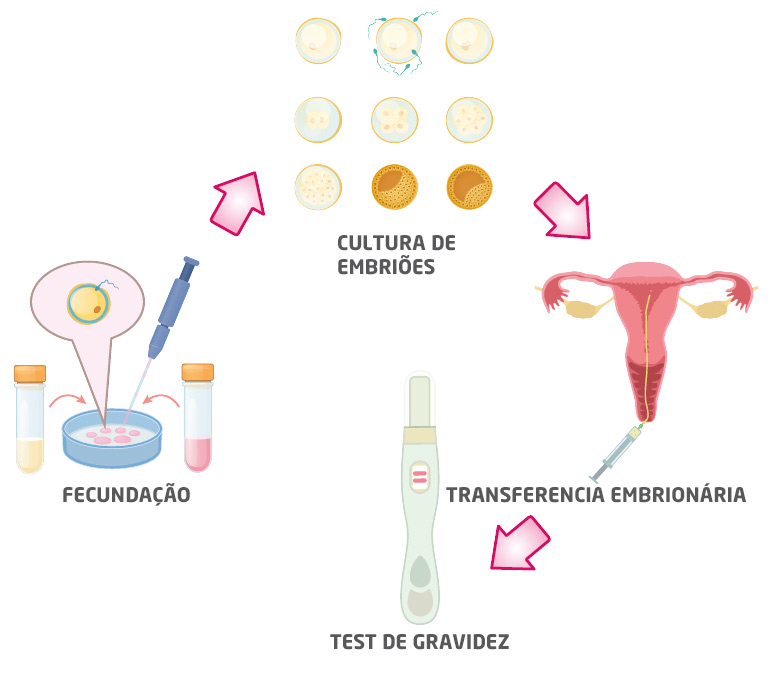
In vitro fertilization: Once the eggs are retrieved, they are processed in the laboratory and inseminated with a prepared semen sample from the spouse or a donor.
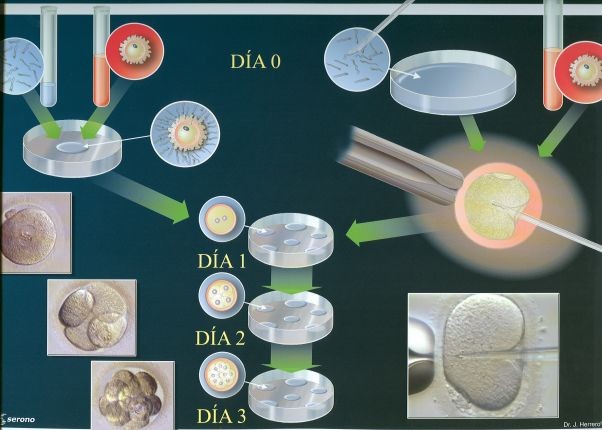
Embryo culture: The day after fertilization (day 1 of embryonic development), the fertilized embryos will remain in culture until they are transferred to the uterus or vitrified, usually until day 5 of embryonic development. At this point in development, the quality of the embryo is categorized based on the likelihood of implantation in the uterus.
Embryo transfer: When embryonic development is adequate, it is transferred to the uterine cavity using a thin catheter guided by ultrasound, or it is cryopreserved by vitrification in case of medical indication or having surplus embryos from the assisted reproduction cycle. This is a simple step that does not require sedation, fasting, or rest to be performed. Portuguese law establishes the transfer of a maximum of 2 embryos, encouraging elective transfer of 1 embryo whenever possible due to the risks associated with multiple pregnancies.
If not enough eggs are obtained after follicular puncture, as often happens in women with low ovarian response or premature ovarian failure, several stimulation cycles can be performed, extracting the maximum number of eggs in each cycle and accumulating (freezing) them until there are enough to perform these techniques with a significant success rate.
The choice of one of these techniques will depend on the couple's subfertility conditions, as well as their reproductive history and the experience of each center.
More about in vitro fertilization
Fertilization
The fertilization process is defined as the fusion of the male and female gametes to form the zygote, which is the first stage of embryonic development.
Fertilization is a physiologically complex process that unfolds over approximately 18 hours. Naturally, it occurs in the fallopian tubes, requiring sperm to reach this region of the female reproductive system after ovulation has occurred. It is estimated that under physiological conditions, between 500 and 1000 sperm are needed to fertilize the oocyte.
The basis of "in vitro" fertilization is to mimic in the laboratory the process that naturally occurs in the fallopian tubes. For this, the oocytes, or more precisely the oocyte-cumulus complexes, are placed in culture plates with fertilization medium and incubated with an appropriate concentration of sperm. The sperm induce the natural disaggregation of the cells surrounding the oocyte (cumulus cells) and initiate the first post-fertilization events. Between 18-22 hours after fertilization, the oocytes are transferred to a new culture medium (without sperm) and the presence or absence of the female and male pronuclei is evaluated under a microscope. The observation of these two pronuclei confirms that fertilization has occurred correctly. Oocytes in which the pronuclei are not observed or that present an abnormal number are discarded as they never give rise to viable embryos.
When the number of motile sperm recovered (REM) is low, the in vitro fertilization process described in the previous section is not efficient. In these cases, a more specialized fertilization technique should be used, which involves micromanipulation techniques to inject a sperm directly into each oocyte. To perform this procedure, the oocytes must be denuded, meaning the cells surrounding them (cumulus oophorus) must be removed using enzymatic methods with hyaluronidase. Once denuded, they are placed in microdroplets, and using an inverted microscope, the oocytes and sperm are micromanipulated using suction and injection needles.
With this technology, it is possible to introduce a single sperm into the oocyte, crossing the zona pellucida (protective film covering the oocytes) and the plasma membrane. Although this technique may seem more invasive, it does not interfere with the normal development of the embryo.
Once the oocytes are microinjected, they are placed back in culture plates suitable for the advanced Time Lapse visualization system, which allows the presence of pronuclei to be verified without disturbing the zygote (fertilized oocyte). The fertilization rate of ICSI is similar to that described for conventional IVF and ranges between 70 and 80%.
Embryonic Development
When the formation of zygotes is carried out in the fertilization laboratory, the development of the embryo must be achieved until the moment of transfer. The embryo transfer can be performed between day 2 after the puncture and day 6. During this period, the cells that make up the embryo divide through a segmentation process until they reach about 32 cells (2-4-8-16-32). At this point, it is called a morula, as its appearance resembles a mulberry. The morula will advance to a more developed stage through a process called cavitation. This embryo with a more complex level of cellular organization is called a blastocyst. In the blastocyst, it is already possible to identify two very distinct structures of the future embryo: a layer of peripheral cells called the trophectoderm (which will give rise to the future placenta) and an inner cell mass (from which the embryo itself will develop).
The development of embryos in the laboratory simulates the natural events that occur in vivo. Currently, it is possible to extend embryo culture time to the blastocyst stage. This advancement is mainly due to the development of new culture media and techniques that have allowed this methodology to be introduced into embryology laboratories in a more routine manner and made available to patients with specific indications.
At IERA, embryonic development is carried out in state-of-the-art incubators with time-lapse technology that allows cinematic monitoring of developing embryos.
At IERA, we work with one of the best, called GERI.
This incubator provides temperature, humidity, darkness, etc., characteristics that are very similar to physiological conditions, and it can be said that the chances of obtaining good embryos and, therefore, achieving pregnancy are much higher than in conventional incubators. Additionally, the image recording system allows monitoring embryonic development without the need to open and close the incubator, further increasing the chances of success without losing relevant information about the entire embryonic development process. Furthermore, patients who wish can receive a video of their embryo.